SADAG
HELPLINE NUMBERS
24-HOUR TOLL-FREE EMERGENCY HELPLINES
Suicide Crisis Helpline
0800 567 567
Department of Social Development Substance Abuse Helpline
0800 12 13 14
SMS 32312
Cipla Mental Health Helpline
0800 456 789
SMS 31393
NPOwer SA Helpline
0800 515 515
SMS 43010
Healthcare Workers Care Network Helpline
0800 21 21 21
SMS 43001
UFS #Fair Kitchens Chefs Helpline
0800 006 333
8AM-8PM TOLL-FREE HELPLINES
Dr Reddy’s Mental Health Helpline
0800 21 22 23
Adcock Ingram Depression & Anxiety Helpline
0800 70 80 90
ADHD Helpline
0800 55 44 33
Pharma Dynamics Police & Trauma Helpline
0800 20 50 26
8AM-8PM SADAG OFFICE NUMBER
SADAG
011 234 4837
WHATSAPP NUMBERS
8AM – 5PM
Cipla Mental Health
076 882 2775
Maybelline BraveTogether
087 163 2030
Ke Moja Substance Abuse
087 163 2025
Have Hope Chat Line
087 163 2050
FOUNDER ZANE WILSON
Contact Founder: Zane@sadag.org
Higher Learning Helplines and Resources

Student and Staff Emergency Contact Numbers - Click here
REQUEST A CALLBACK

Request a Callback from a Counsellor
Click here
SUPPORT GROUPS
SADAG has over 160 free Support Groups. To find out more about joining or starting a Support Group click here.
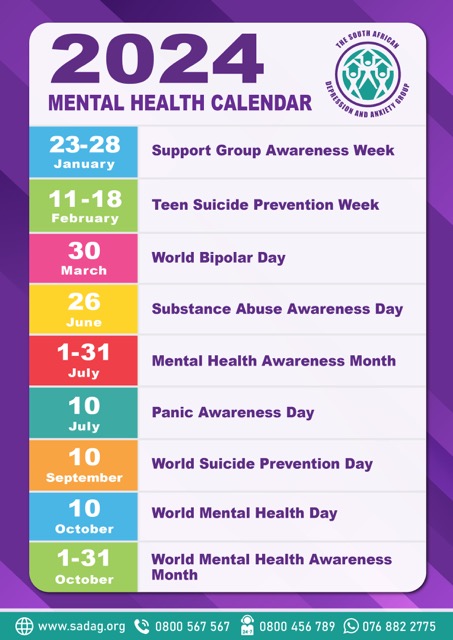
Mental Health Calendar 2024
To view our Mental Health Calendar
click here