November 2003
Medical aids’ step “biggest disaster” for mental health in years
THE SUDDEN move by medical aid schemes to deny chronic medication benefits for various mental illnesses has been condemned as the “biggest disaster to hit psychiatric care in South Africa in the last 10 years”.
The arbitrary and unilateral move, which could endanger the lives of thousands of sufferers across the country, has drawn widespread criticism from leading groups involved in mental healthcare including the SA Depression and Anxiety Group (SADAG) and the healthcare consumer watchdog, Rights Education and Activism for Consumer Healthcare (REACH).
“People suffering from Bipolar Mood Disorder (BMD, previously known as manic depression) and depression are particularly at risk,” says Zane Wilson, founder of SADAG.
“As with numerous physical diseases such as hypertension, sufferers of BMD and depression can and do function as productive contributors to the economy and highly capable members of society at large. But this is only possible with continued proper medication and monitoring.
“Without regular medication, sufferers not only risk serious regression with resultant personal setbacks and even hospitalization, but more dire consequences including suicide and even violent attacks,” says Wilson.
Nusreen Khan, national co-ordinator of REACH, slammed medical schemes for “shirking their moral responsibilities and making a mockery of legislation governing medical schemes”.
Outraged patients, many of them successful business leaders and heads of families and whose conditions have stabilized under consistent treatment, have inundated SADAG and REACH with complaints.
“The Council for Medical Schemes is basing the lack of published guidelines for the treatment of BMD on the fact that too few medications are registered. This does not take into account the thousands of patients who are stabilized on current medication,” says Khan.
“It is understandable that treatment guidelines need to be structured on solid evidence-based data. One needs to take into account that, even though certain medications might not be registered in SA, they are however registered abroad. The consequences of the slow registration process for medicines in SA are being borne by patients here.
“We cannot understand how an industry, funded by consumer money, refuses to consult with those very consumers. Instead they discuss critical issues affecting the very lives of their members in clandestine cabals and then, insensitively and callously notify members that they have decided to pull the rug out from under them.
“Although BMD has been included in the list of so-called ‘25 prescribed minimum benefits (PMB)’ conditions for chronic medication, individual schemes are refusing to cover costs on the grounds that no treatment protocol exists for BMD.
“In effect, this verbal sleight-of-hand means there are only 24 PMBs, excluding bipolar mood disorder,” says Khan.
REACH approached the Council of Medical Schemes to assist in drawing up guidelines regarding mental healthcare benefits, “but, in essence, we were told we would be contacted if our inputs were needed. It was a case of don’t call us, we’ll call you.
“They never called,” says Khan.
“In a bizarre twist, these illnesses, including BMD, are still recognized as chronic diseases – just not funded any more. Medical schemes are not legally bound to reimburse patients for medications for BMD. There should be very specific guidelines underpinning the lack of a protocol for the treatment of BMD. For example, patients stabilized for a specific period of time should be reimbursed by their medical scheme.
Depression is acknowledged as the world’s second biggest cause of adult deaths, and BMD causes violent mood swings, ranging from feelings of euphoria to abject despair.
Previously known as manic depression, BMD sufferers may fall into a manic state resulting in extreme violence and even homicide if their condition is untreated.
“The potential for catastrophe is very real,” warns Khan.
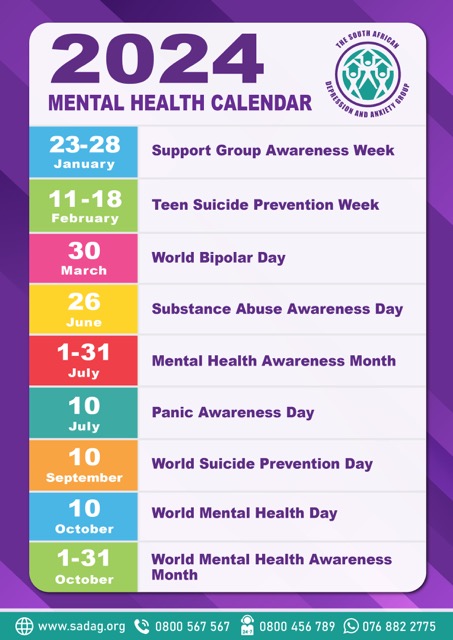
“It comes as a major disappointment to us at SADAG, especially after several encouraging advances in mental healthcare in recent time,” says Wilson. “We have made important advances in bringing mental illness out of the closet, in addressing the crisis of the growing number of teen suicides, in interacting with global funders such as the World Bank and even saw nationwide focus on the mental health issues on 10 October - World Mental Health Day.
“This unilateral and impassible step is a serious setback for all the good we have done to date. Because so much stigma still lingers around mental illness as distinct from physical illness, extra care must be exercised in the diagnosis and treatment of diseases such as BMD and depression.
“This kind of draconian step by medical schemes only aggravates the situation. That it was taken without any consultation whatsoever is unconscionable,” says Wilson.
In addition to the spectre of having to spend hours in queues at state hospitals, thousands of people on chronic medication now have to thread their way through a veritable labyrinth of different interpretations, conditions and sub-conditions and a host of “products” within individual medical schemes.
“This sort of hostile environment serves only to alienate sufferers and place potentially disastrous stress on people whose ability to cope is at best tenuous. We cannot understand how medical schemes reached such an illogical and insensitive crisis. We will pursue every means available to get them to reconsider,” say Wilson and Kahn.